Some researchers have said that red meat leads to colon cancer. In 2015, the World Health Organization (WHO) proclaimed that red meat was a Class 2 carcinogen, and that processed meat was a Class 1 carcinogen, which puts it in the same category as smoking cigarettes in terms of the risk of developing colon cancer. The level of relative risk was around 17 percent for red meat and 18 percent for processed meat.
Scientists from all over the world have criticized this proclamation for several reasons. Independent observers of the process that the International Agency for Research on Cancer (IARC) used to inform the WHO’s declaration have pointed out that it was not a consensus decision because approximately 30 percent of the participants disagreed. About 800 studies were considered, but only about 50 were deemed worthy of supporting the position that meat causes cancer; the other studies were thrown out for various reasons.
Dr. Georgia Ede has done a remarkable job of sorting through the same data that the IARC cited, and she has determined that the evidence in support of the claim that meat causes cancer appears to be fairly underwhelming. You can find Dr. Ede’s critique at DiagnosisDiet.com, and it’s well worth reading. To summarize, her findings show that the vast majority of the data comes from epidemiology, which always lumps true meat eaters with those people who eat junk like burgers, shakes, and fries.
Much of the other research was based on rat studies in which the animals were genetically bred to develop cancer, given a cancer-inducing drug, and then fed meat and some toxic rat chow. These types of studies are hardly applicable to a normal human being who eats a healthy diet that includes meat, and the studies in no way accurately represent the habits of a purely carnivorous human. Among those studies on rats and mice were a majority that didn’t support the hypothesis that meat causes cancer, and there even exists a study that concludes that bacon was relatively protective against colon cancer. Dr. David Klurfeld, who was one of the IARC panel members, has recently spoken out about the process. He was fairly concerned that contradictory evidence was dismissed and that a large percentage of the panelists were vegan or vegetarian but did not disclose that information on the review.
Let’s assume that the weak evidence that the WHO used was sufficient to suggest a true relative risk increase in cancer of 18 percent. What does that mean? Well, the generally accepted lifetime risk of developing colon cancer is about 4 percent. If the WHO is correct, that risk goes to 5 percent. In other words, based on the data that supports the WHO’s claim, there’s a whopping 1 percent increase in absolute risk. This is one of the classic statistical numbers games used to scare people from consuming something that someone doesn’t like for various reasons. As always, meat consumption is not the only factor in the risk of developing cancer; we also could look at things like hyperinsulinemia, abdominal obesity, and chronic inflammation (and we could paint a far scarier picture).
As I see it, there are two possible approaches to the WHO’s decree: You can question the findings of the WHO because of the poor science backing them, or you can put the findings in context with other factors to determine your overall risk. People who follow a carnivore diet often report greatly improved insulin status, lower levels of abdominal obesity, and significantly reduced inflammation. When you put the whole package together, you find that overall risk for colon cancer likely falls for people on a carnivore diet. Remember—when we talk about associational data, you always should ask, “Does this apply to all people in all situations?” Rats that have been genetically bred to develop cancer and have been given a drug that promotes cancer shouldn’t chase down a bolus of toxic rat chow with a steak. Similarly, people who spend their lives eating sugar, vegetable oils, and refined grains and become insulin resistant and obese may want to avoid triple bacon burgers with a side of fries and a shake.
In Asia, red meat and processed meat (whether cooked or raw) has basically no association with colorectal cancer. Is meat on that continent magically different than in North America? Not likely, especially because much of the red meat in Asia is imported from the United States. Do the Asians have special meat-resistant genes? That’s also not likely because when Asians emigrate to the United States, the likelihood that they’ll become sick and fat and develop cancer goes up. Instead, perhaps the higher incidence of colorectal cancer in North America has to do with the garbage that we eat with our meat rather than with the meat itself. (Note: Only about 4.5 billion people live in Asia, so I’m sure it’s totally fine to ignore their data.)
Excerpted from The Carnivore Diet, By Dr. Shawn Baker.
Learn more HERE
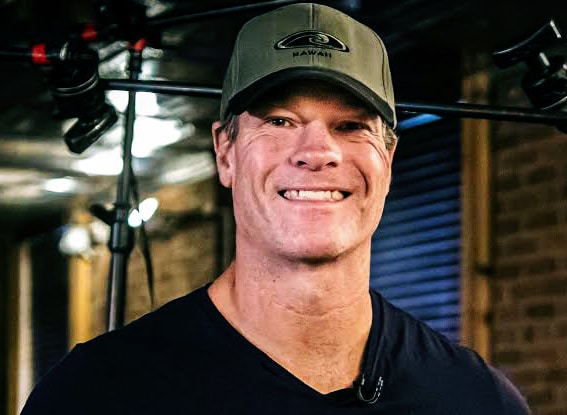
Reviewed & approved by
Dr. Shawn Baker, MD & Carnivore.Diet team.

1 thought on “The Red Meat Cancer Risk Doesn’t Add Up”
Excellent and especially easy to understand. You guys are doing a great job.
Art in Nashville